Overcoming Chronic Pain
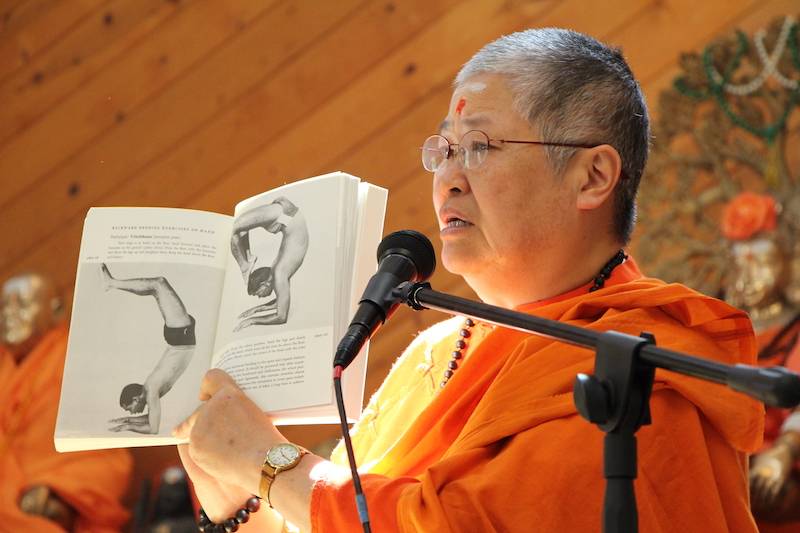
by Swamisankariananda

Swami Sivasankariananda
SF Sivananda Center Director
Swamiji took sannyas in 2017 and is a certified yoga therapist. She co-teaches Sivananda Yoga Teacher Training Courses and Sivananda Yoga Health Education Trainings and focuses on teaching Chronic pain management.
Pain is the main reason people go to the doctor. Unfortunately, 20% of American adults suffer from moderate to severe chronic pain , as do 13% of North American teens and 10 to 30% of the adult population of Europe.
Its effects are physical, psychological and spiritual. Acute pain is typically a pain with a specific, identifiable cause, and a pain like twisting your ankle that resolves relatively quickly. Additionally, pain becomes chronic when it lasts three to six months.
Chronic pain can stem from an acute injury or surgery, but doesn’t always. The most expensive pain conditions in America are headache, arthritis and back pain. Furthermore, it can affect daily activities such as work, relationships, and sleep.
When pain is persistent, it can lead to mood disorders, depression, even suicide. Recent research suggests that pain can affect the chemistry of the brain and the functioning of the nervous systems.
Other people, including many doctors, may find it hard to believe the severity of persistent pain. (The choice of the word “persistent” is intentional, as “chronic” does not sound hopeful!)
Pain is subjective
How can we really know how much pain someone is in? It is very difficult to describe or measure. “On a scale of 1 to 10, how bad is your pain?” How can we know whether one person’s 8 out of 10 is the same as another’s 8 out of 10?
It is the same conundrum as trying to explain color to a blind person, or trying to describe the taste of jackfruit to someone who has never tasted it. We can try using adjectives like “aching,” “burning,” “sharp,” “shooting,” “radiating,” but these are also imprecise.
Our capacity to communicate about pain is equal to the challenge of describing what love feels like, and how deeply impacting it is.
Protective Response
The human body comes equipped with many protective mechanisms—among them are sneezing, muscle spasms, the fight/flight response… and pain.
Pain is a normal human experience, ensuring our survival. Its job is not only to alert us to danger, but make us stop what we’re doing, move away from the danger and sometimes even go lie down. Imagine the members of the Marsili family in Italy; because of a rare genetic mutation, they feel little or no pain.
That might sound good at first, but consider the potentially dangerous consequences. You could burn yourself or break a bone without knowing it. You could then keep moving and make matters worse.
What is Pain?
Recent advances in pain science focus on the nervous system and the brain. The central nervous system consists of the brain and spinal cord. The peripheral nervous system consists mainly of nerves. When something potentially harmful happens, a message is sent to the brain via nerves and the spinal cord.
Note that the impulse sent is not a pain message, but a danger message. (Neurons cannot tell the difference; they just relay a signal.)
Three things excite the neurons in your pain-danger system: mechanical forces on your tissues, chemical irritations and extremes of hot and cold. The greater the perceived threat, the more neurons jump into action, the more insistent the message.
It is not until the information from the senses reaches the brain, though, that a decision is made about how dangerous it is and whether something needs to be done.
But the pain we feel is not an accurate indication of tissue damage or health. A major injury might not hurt much and a small paper cut can hurt a lot. The brain also deals with information presented on a priority basis. And that is a decision between it and you.

Nervous System: Experience, Not Facts
Nerves are made up of thousands of nerve cells, or neurons. They sense information and send messages via electrical impulse. If the message is loud enough and travels the length of the neuron, the neuron releases chemicals to excite the next neuron.
The chain reaction reaches the spinal cord. If an immediate response is needed, a reflex can be initiated from there. Otherwise, signals may be amplified and sent along to the brain. The brain provide us with experiences, not facts.
The signals lead to brain activity that creates pain. Action impulses from the brain can then influence any system of the body. Usually long before tissue heals, the brain itself reduces the danger signals and its own response, allowing pain to subside so “normal life” can resume.
Pain is Complex
There are 45 miles (72km) of nerves in the body, all collecting information about what is happening inside and outside the body. In the brain alone, there are 100 billion nerve cells. That’s 1,000 trillion connections passing information around the brain.
Pain Can Persist after Tissue Heals
There are cases where, after three to six months, the tissue may have healed, but the pain remains. Many systems have gone on red alert, usually including the emotional systems. Fear and worry feed right back into pain, revving it up. It is harder to pay attention.
Less endorphins, and other feel-good chemicals, are being produced by the brain when there is pain. It becomes harder to feel anything but pain in the body, harder to plan refined movements. Pain can lead the person experiencing it into a spiral—into a lonely, desperate, even life-threatening position.
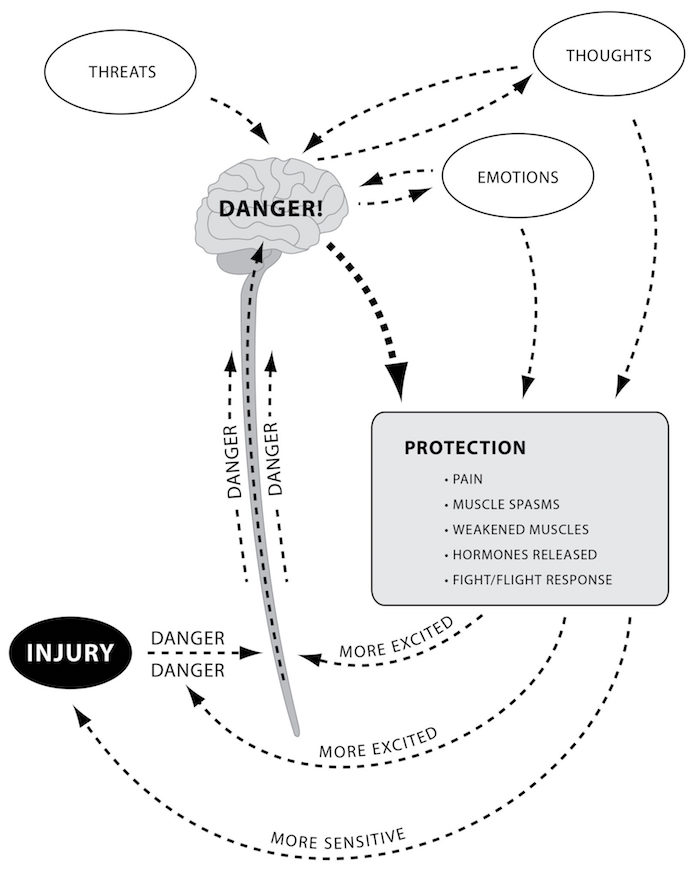
Revving up the fight/flight response. Courtesy of Neil Pearson
The Nervous System Gets Wound Up
Persisting pain is related to two things: 1) changes in the physical body; and 2) neuroplastic changes in the nervous systems. Pain can get worse because the nervous systems decide to pay closer attention to the danger signals. Excited neurons send even more signals, exciting neighboring neurons.
The threshold of the neuron sensors are lowered. With this much activity, the neurons function as if there is considerable danger and begin to produce inflammation to protect the body. The nervous system is wound up. The neural pathways related to pain expand.
Similar changes of wind-up happen in the brain, and it can seem that positive feedback loops build allowing the changes to create a story of considerable danger, which then loops back to create more pain and more sense of danger. Research shows that understanding this process can help reduce pain.
[“Suffering equals pain multiplied by resistance.” —Shinzen Young]
Pain takes over other functions
When pain is experienced, 200 to 400 parts of the brain can get excited. The pain alarm system becomes hypersensitive. Normal functions of the brain in those areas are altered—some more active and some less. The pain can seem to spread as the signal expands into adjacent areas of the brain.
Day-to-day activities such as thinking, planning and regulating emotions can be impacted. While pain might normally be processed in 5% of the nerve cells in a particular area of the thinking brain, in persistent pain, it can expand to 15–25% of the cells. The brain learns pain.
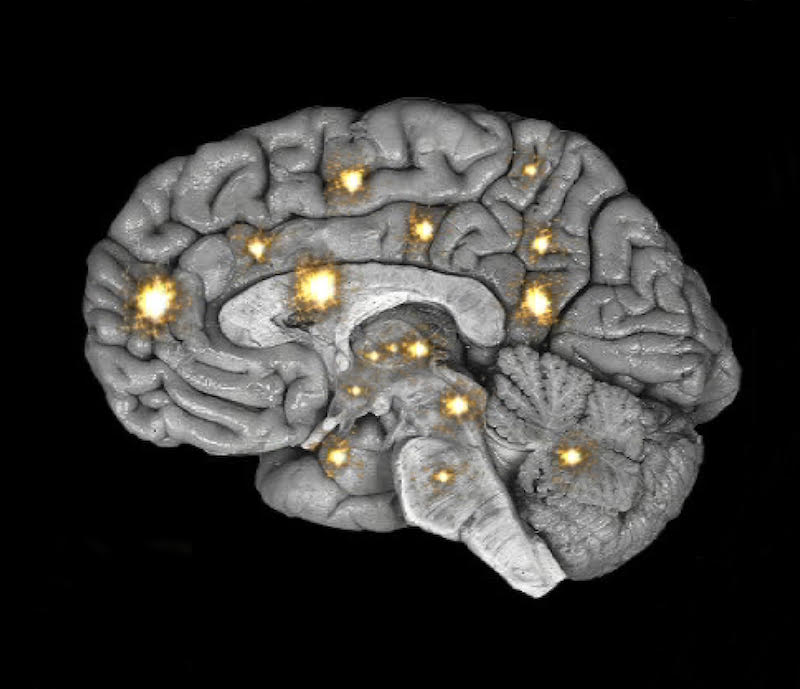
Many areas of the brain can light up when there is pain.
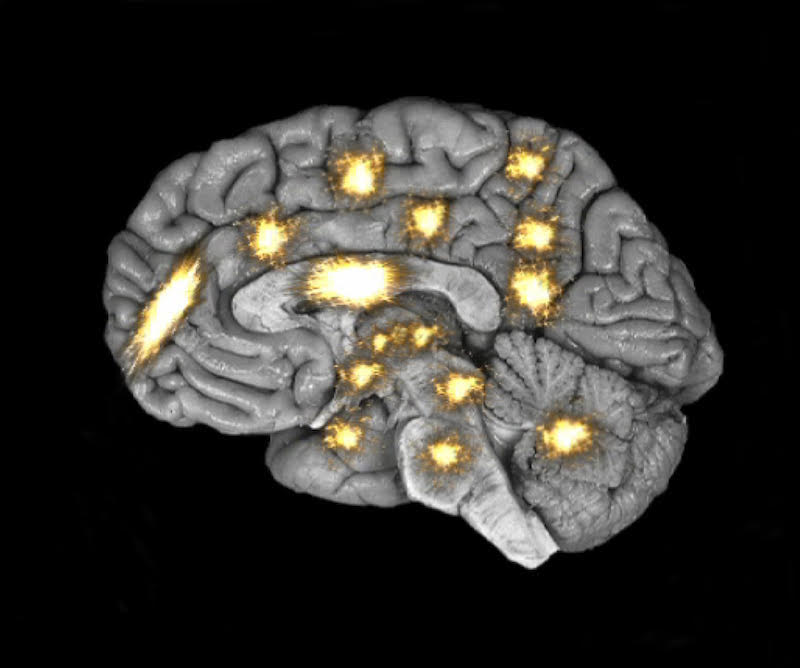
If the pain becomes chronic, more of the brain is processing it and the lit area grows.
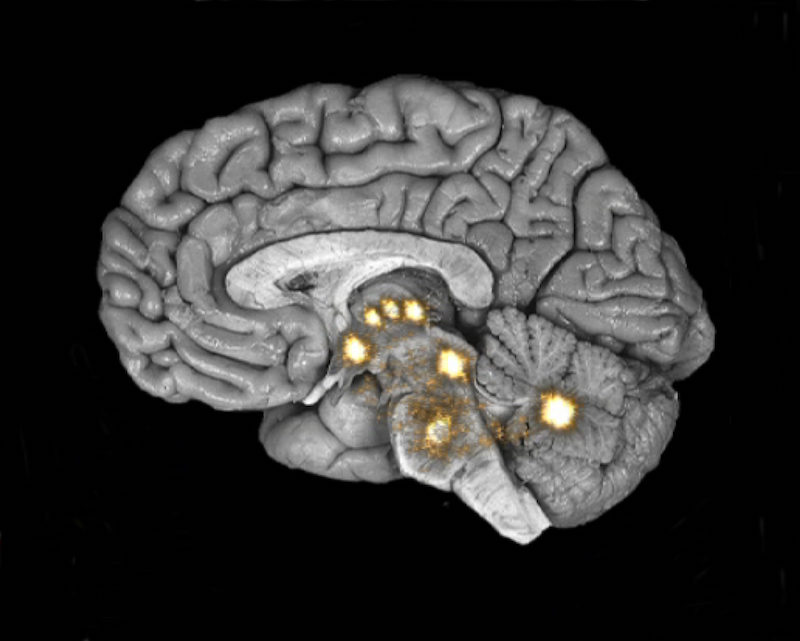
When the signals subside, no more pain.
Courtesy of Michael Moskowitz, M.D. and Marla Golden, D.O. and the neuroplastix.com website
The Body Map/Subjective Memory
The brain relies on being able to feel the body. It “sees” the body differently than we see ourselves. Given the large number of nerve endings in the skin, the brain receives more detailed information about the skin than what’s inside it. The more information, the bigger that body part becomes in our internal “body map.”
Pain distorts how the brain perceives the body (as do memories, anxiety, preconceived ideas, etc.). A person with hand pain, may literally experience the hand being larger than normal.
We may experience joint stiffness or pain; in actuality, the problem is in the nervous systems, not only in the body. The brain is sending the wrong signals. More things trigger the pain, even the slightest stress.
You Can Change Pain
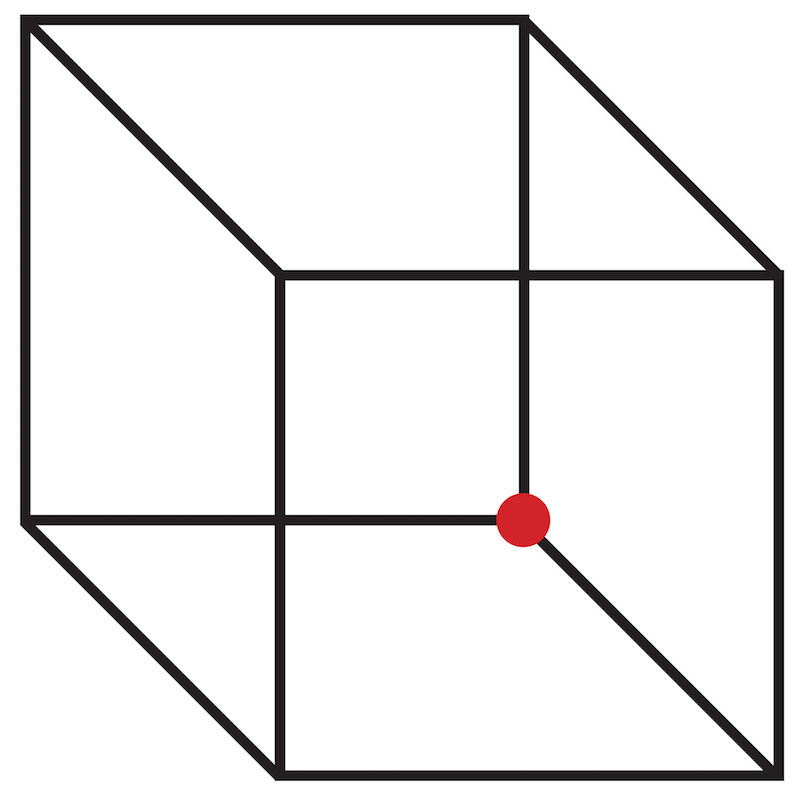
Is the red dot inside or outside the cube? If you can change how you see this cube, that means you can change how you perceive visual inputs to your brain. And if you can do that, do you think you can change how your brain perceives danger signals?
If we are too quick to run from pain, or medicate it, we miss what it is trying to tell us. If we allow the battle to be between the doctor and the disease and think the solution is outside ourselves, we never get a chance to find the inner resources to face the situation, or find our own solutions to the problem. When we work together with Nature, different outcomes are possible.
What is Neuroplasticity?
The good news is that the nervous system is adaptable and constantly changing. Nerve cells in the brain change connections and behavior when new information is presented. One function of the brain can be transferred to an adjacent area of the brain if needed.
If someone is blind, the areas of the brain that process visual information are free to process information from other senses. Thus there can be heightened awareness in other senses. If we don’t exercise a brain function, our potential in that area decreases. Equally, we get better at whatever we practice.
- Education in pain neuroscience can help put the ball in our court. The nerves will learn whatever we practice. Thanks to neuroplasticity, we have the power to influence how the nervous system functions. It is not necessarily easy or quick, but it is feasible.
- Neurons can be changed by almost anything—how we move, by input through our skin, how we stretch, what we think, what we see, our environment, what we believe, our emotions, etc. We have the ability to change each of these things, so we have considerable power to change how our neurons work
- Sensors at the end of nerves are replaced every few days. We have some influence on the sensitivity of the new sensors. Given that there are trillions of sensors in your body, and thousands are replaced every second.
“More time in a calmer state, more opportunity for positive change.” —Neil Pearson
Every second your nervous system is in a state of more calmness, your body has the opportunity to replace the highly sensitive ones with the more normal (low sensitivity, high threshold) sensors.
- Brain chemistry changes when we practice finding ways to be happier. The fight/flight response causes the release of cortisol, which leads to more pain. Endorphins are produced when we are more content. Older adults with arthritis who are in good marriages experience less pain than those who are single or in unsupportive relationships.
- According to Neil Pearson, “One endorphin molecule may be able to block as many as 50 danger signals.” This makes endorphins even more powerful than morphine—but with pleasant side effects.

Keep Moving
Movement is an essential approach for successful pain care. The hypersensitive nervous systems are wary of movement, though. We move tentatively and an internal warning alarm comes on—even before there is any real danger— so we stop.
However, to work towards regaining ease of movement, we must first be calm and attentive, then move up to and just beyond the edge of the pain. As the alarm goes off, ask, “Is it really dangerous? Will I regret it? Maybe this is just a normal situation.”
By challenging the alarm, we turn it down. Muscles need to be taught that it’s okay to move and stretch. We must reconnect with body sensations, paying more attention to them than to the pain.
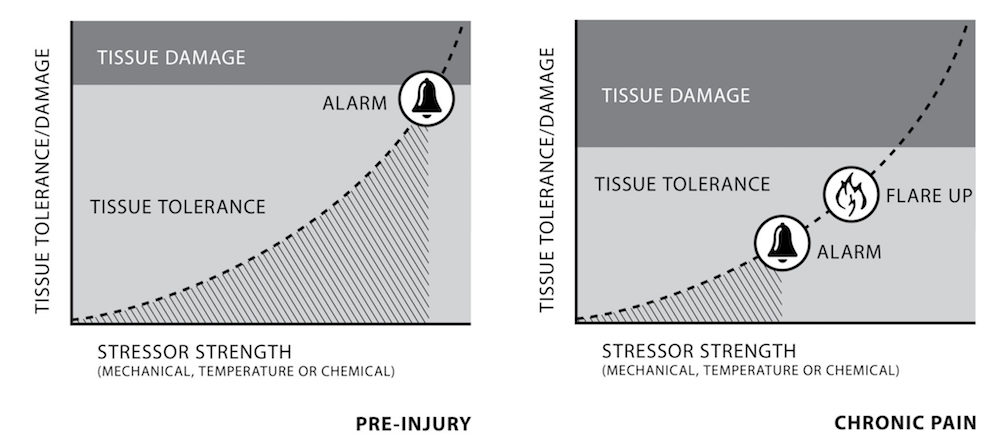
The body will protect you from tissue damage. Once there is chronic pain, the warning alarm comes on prematurely. We believe there is danger sooner, so we give in to the alarm. Mobility decreases.
Courtesy of Neil Pearson
How Yoga Helps
Pain can be changed. And so can suffering associated with pain. Pain does not have to equal suffering. All is changing. Pain will change. In Yoga we learn to observe, accept what is and do our duty, putting aside personal preference. The experience is not about pain, it is what is behind the pain that brings insight into deeper truths. We go beyond our limited idea of self and expand.
Used as a therapeutic treatment, yoga helps relieve pain and muscular tension, fostering greater ease of movement and building self-reliance. Physical, mental and spiritual self-awareness and self-regulation improve. Feelings of anxiety, fear and isolation are reduced and a better quality of life can be found. It is accessible, less costly than medical intervention and has long-lasting effects—setting us on the journey to connect with the holistic Self, highest Self, the Perfect Self.
The five points of Yoga are the best medicine:
- Proper Breathing – Conscious breathing winds down the nervous system. An effective way to trigger parasympathetic response and release endorphins before moving is the following simple exercise. Just practicing this three to five times a day can help regulate the nervous system.
Longer, Smoother, Softer Breathing Practice
In any comfortable position, focus on your breathing. It doesn’t have to be any particular way, just watch it for a minute or so. Next, see if you can make it a little longer. Observe for another minute. Then, see if you can make it a little smoother. Observe. Finally, can you make it a little softer?

Savasana is an optimal position for body awareness practice.
- Proper Relaxation – It is difficult not to focus on pain when it is severe. It is also challenging to relax. Practice a body scan in savasana (or sitting, if it’s more comfortable) to build body awareness.
Body Awareness Practice
Starting with the feet and toes, pay attention to any subtle, non-pain sensations. Take your time and go through the entire body. This can prepare you to move calmly into an adapted yoga sequence with ease and confidence.
• Proper Exercise – Mild to moderate exercise can decrease physical pain. Monitor muscular tension. Take note of how the breath feels, how the mind feels, how the spirit feels. Stay calm. Do not ignore pain. Be sure you feel safe. The yoga sequence should be gentle and at a slow pace.
Slow, Gentle and Conscious Asana Practice
Pause to take a slow, deep breath between rounds of sun salutations. When practicing bhujangasana, for instance, inhale up and exhale down a few times with no long-holding.
Continue to monitor the body/mind/breath. Stop any time you cannot maintain the state of calm. Progress slowly.


• Proper Diet – The yogic (vegetarian) diet can help reduce pain and inflammation, and can even help reduce side effects of medications.
Anti-Inflammatory Diet
Eat lots of vegetables, beans, fruits and a variety of whole grains. Include nourishing fats and high-quality protein.
Use ginger and turmeric. Restrict dairy and grains. Reduce flour and sugar intake. Avoid nightshade vegetables—potatoes, tomatoes, peppers and eggplant and processed food.
• Positive Thinking and Meditation – Thought, like proper movement, is among the most effective ways to stimulate neurons in the brain circuits. The mind drives pain. The mind can also reverse it. Imagine an area of the brain devoted to pain is shrinking. Reframe stressful events as beneficial.
“Pain” can be rephrased as “sensation.” Cultivate less fear responses. In working with the mind, we gain the ability to focus for longer periods. We can manage stress. Positive thinking produces endorphins. We build self-awareness, quiet the mind and senses. In a 2011 study using functional MRI results, four hours of meditation training was shown to significantly reduce pain intensity.


Yoga is Medicine
Highly effective self-care, Yoga requires the utmost patience and perseverance. By its steady practice, we can not only change pain, but empower people to live with joy and meaning. We seek to cultivate the same awareness in meditation practice, leading to the non-dual state where there is only peace; pain disappears.
—Swami Sivasankariananda
With gratitude to Neil Pearson, a Canadian physiotherapist, professor and yoga therapist, who is extremely generous with his significant wisdom regarding the latest advances in understanding pain.
This article was reproduced and edited from Sivananda Yoga Life magazine, spring/summer 2018 issue. No part of this article may be reproduced in any form without the written permission of the author.
Yoga Teacher Training Course
Check out our 200-hour Yoga Alliance certified Yoga Teacher Training Courses offered twice a year in California, 3x in Vietnam, once in China and once in Japan.
Foundational Courses
Choose from upcoming courses for beginners and intermediate level students.
Yoga Vacation
Rejuvinate your body and mind. Experience and progress with daily Yoga classes. Learn the 12 basic asanas and pranayama. Enjoy daily meditation, chanting, and organic vegetarian meals.
Rejuvenate Your Being
A Yoga vacation is an ideal getaway to change perspective towards one’s life and become healthier, more relaxed and connected.


0 Comments